The Iron Lung Machine and Its Role in the Fight Against Polio
The iron lung machine, a medical marvel of its time, played a pivotal role in the treatment of polio, particularly during the mid-20th century when polio outbreaks were at their peak. For many, the iron lung was a life-saving device, providing a means of survival when respiratory muscles became paralyzed due to the devastating effects of the poliovirus.
This article delves into the history of the iron lung machine, how it worked, and its significance in the fight against polio.
What is Polio?
Poliomyelitis, commonly known as polio, is a viral infection that can lead to severe consequences, including paralysis and even death. The poliovirus primarily affects young children, and in severe cases, it attacks the nervous system, resulting in muscle weakness and paralysis. When polio affects the respiratory muscles, individuals lose the ability to breathe on their own, a condition that can be fatal without medical intervention.
Polio Epidemics of the 20th Century
In the early to mid-20th century, polio epidemics were rampant across the world, especially in developed countries. The 1940s and 1950s were particularly notorious for large-scale polio outbreaks. Thousands of children were left paralyzed or struggling to breathe, and the demand for a solution grew urgent. Before the widespread availability of the polio vaccine developed by Jonas Salk in 1955, the iron lung was the primary tool to support patients with paralyzed respiratory muscles.
The Iron Lung Machine: A Life-Saving Invention
The iron lung machine, also known as a negative pressure ventilator, was invented by Philip Drinker and Louis Shaw in 1928. This cylindrical device was designed to assist patients with respiratory paralysis, providing artificial respiration by creating a negative pressure environment around the body.
How the Iron Lung Worked
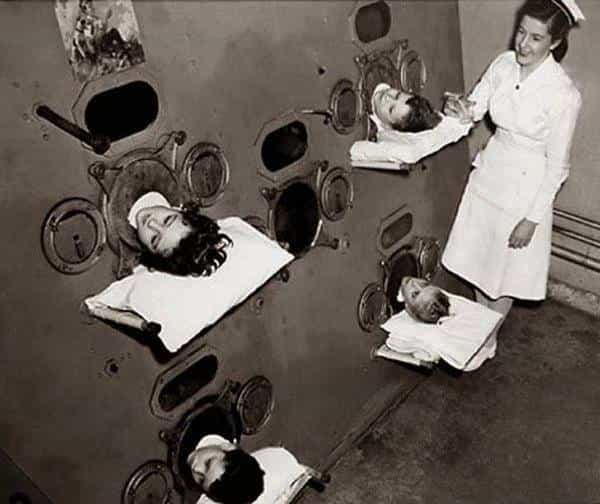
The iron lung was essentially a large, airtight metal cylinder in which a patient would lie. Their body, from the neck down, was enclosed in the machine, while their head remained outside. The machine operated by manipulating air pressure within the chamber.
– Negative Pressure: When the machine expanded, it created a vacuum that caused the patient’s chest to rise, mimicking the natural process of inhalation. Air was drawn into the lungs as a result.
– Positive Pressure: When the machine contracted, it increased the pressure in the chamber, forcing air out of the patient’s lungs, simulating exhalation.
By alternating between these two phases, the iron lung allowed polio patients with paralyzed diaphragm muscles to breathe. This method of mechanical ventilation saved countless lives at a time when no other option was available.
Iron Lung and Polio Patients
During the height of the polio epidemics, many hospitals across the United States and other affected countries had entire wards filled with iron lung machines. Patients could remain in these machines for weeks, months, or even years, depending on the severity of their condition. For those suffering from respiratory paralysis, the iron lung provided the only means of survival until their muscles could potentially recover enough to breathe independently.
Living in an Iron Lung
While the iron lung was a remarkable invention, life within the machine was far from easy. Patients were confined to the device, unable to move freely, and completely dependent on it for breathing. Despite the challenges, many patients adapted to life in the iron lung, with some individuals spending decades inside the machine.
One well-known case is that of Martha Mason, who lived in an iron lung for over 60 years following a bout of polio as a child. Her resilience and ability to lead a productive life despite being confined to the machine is a testament to human endurance and the crucial role the iron lung played in polio treatment.
The Decline of the Iron Lung
The invention of the polio vaccine in the 1950s marked the beginning of the end for the iron lung. As vaccination campaigns became widespread, the incidence of polio dropped dramatically, and the need for iron lungs decreased. By the late 20th century, iron lung machines were largely replaced by more modern and portable ventilators.
Modern Alternatives to the Iron Lung
While the iron lung has become a relic of the past, advancements in medical technology have produced more efficient and less cumbersome respiratory support devices. Today, positive pressure ventilators, which work by pushing air directly into the lungs through a mask or tube, are the standard for patients with respiratory failure.
Although iron lungs are no longer widely used, a few still remain operational, primarily for patients who have lived in them for most of their lives and cannot easily transition to newer devices.
The Legacy of the Iron Lung
The iron lung machine remains an iconic symbol of the fight against polio. It represented hope for thousands of families and patients affected by the virus, and its impact on medical history cannot be overstated. While modern medicine has moved past the need for such devices, the iron lung is a reminder of the immense challenges posed by polio and the life-saving innovations that helped overcome them.
The Importance of Vaccination
The story of the iron lung is a powerful reminder of the importance of vaccination in preventing deadly diseases like polio. Thanks to widespread vaccination efforts, polio has been nearly eradicated globally, and the iron lung is now mostly a historical artifact. However, the lessons from the past continue to inform present-day public health strategies and emphasize the need for continued vigilance in disease prevention.
The iron lung machine played a crucial role in the battle against polio, providing life-saving support to patients during some of the worst polio outbreaks in history. Its legacy lives on as a testament to human ingenuity and the importance of medical advancements in combating infectious diseases. Although the iron lung has been replaced by more modern ventilators, it remains a symbol of resilience and hope in the face of overwhelming odds.
FAQ related to the iron lung machine and polio:
1. What is an iron lung machine?
The iron lung is a type of mechanical ventilator that was used to help polio patients with respiratory paralysis breathe. It works by creating negative and positive pressure to mimic the natural breathing process.
2. How does the iron lung machine work?
The iron lung operates by alternately creating a vacuum (negative pressure) and releasing it (positive pressure) in an airtight chamber around the patient’s body, forcing the lungs to inflate and deflate, helping the patient breathe.
3. Why was the iron lung used for polio patients?
Polio can cause paralysis of the respiratory muscles, preventing patients from breathing on their own. The iron lung provided a way for those with respiratory paralysis to breathe when their muscles were not functioning.
4. When was the iron lung invented?
The iron lung was invented in 1928 by Philip Drinker and Louis Shaw, initially as a means to support patients with polio-related respiratory failure.
5. Why is it called an “iron lung”?
The machine is called an “iron lung” because of its large metal (iron) body that enclosed the patient, except for the head, and its function as an artificial lung for breathing.
6. How long did people live in an iron lung?
Some polio patients lived in iron lungs for weeks, months, or even decades, depending on the extent of their respiratory paralysis. A few people have lived in iron lungs for the majority of their lives.
7. Is the iron lung still used today?
The use of iron lungs has been almost entirely phased out due to the development of more modern ventilators and the eradication of polio in most parts of the world. However, a few individuals who have spent most of their lives in iron lungs continue to use them.
8. What replaced the iron lung?
Modern positive pressure ventilators, which deliver air directly into the lungs via a mask or tube, have largely replaced the iron lung. These devices are much smaller and more efficient.
9. What role did the iron lung play during polio outbreaks?
The iron lung was a critical life-saving device during polio epidemics, especially in the 1940s and 1950s. It was the only way to keep patients alive when their respiratory muscles were paralyzed by the virus.
10. Did the invention of the polio vaccine eliminate the need for the iron lung?
Yes, the polio vaccine, developed by Jonas Salk in 1955, significantly reduced the number of polio cases, leading to the eventual decline in the need for iron lungs.
11. Are there any famous people who lived in an iron lung?
Yes, Martha Mason is one of the most well-known individuals who lived in an iron lung for over 60 years after contracting polio. Her story is often cited as an example of resilience in the face of adversity.
12. What is the legacy of the iron lung?
The iron lung is remembered as a groundbreaking medical invention that saved thousands of lives during the polio epidemics. It symbolizes the challenges of dealing with infectious diseases before the development of vaccines and advanced medical technology.
13. Where can I see an iron lung today?
Iron lungs can be seen in some medical museums and history exhibits that showcase the history of medicine and the fight against polio. Some old machines are still in private use by patients who rely on them for breathing.
14. How did patients eat or drink while in an iron lung?
Patients in an iron lung could eat and drink normally, though it required assistance. Their heads were outside of the machine, and they were often fed by caregivers through straws or other assisted methods.
15. Why isn’t polio as much of a problem today?
Polio has been nearly eradicated thanks to widespread vaccination efforts, making it a rare disease today. Countries around the world have adopted vaccination programs to prevent its spread, eliminating the need for devices like the iron lung.
